Abstract
Introduction
Outpatient autologous stem cell transplantation (ASCT) has become standard of care in many centres due to limited inpatient resources and rising financial constraints. Outpatient ASCT involves family members/friends assuming patient care responsibilities during the acute transplant period. Although this may be associated with reduced direct medical costs, less is known about the "out of pocket costs" and "lost opportunity costs" to patients and their caregivers, as well as impact on caregiver quality of life (QOL). Outpatient transplantation is perceived to provide superior QOL for patients, but there is little evidence to support this. Thus, our objectives were to compare the QOL of patients and their caregivers undergoing outpatient and inpatient ASCT, and to quantify indirect costs to them.
Methods
This is a single centre cohort study of patients with lymphoma and multiple myeloma undergoing ASCT at Princess Margaret Cancer Centre from April 2016 - February 2021. Patients without a primary caregiver were still eligible to complete the QOL portion of the study. Patients completed several questionnaires including FACT-BMT, FACT-F, and EQ-5D. Caregiver questionnaires included: Caregiver Quality of Life Index-Care (C-QOLC), and a caregiver self-administered financial expenditure survey (C-SAFE). Total indirect costs were defined as lost opportunity costs (i.e., wages) plus out-of-pocket costs (e.g., parking, accommodations). Questionnaires were completed at 5 time points: D0 (prior to ASCT), D+7, D+14 (discharge from daily visits), D+28 (discharge from ASCT) and D+100 (follow-up). Demographic and clinical characteristics were assessed using descriptive statistics. Pairwise changes in QOL from baseline were assessed using linear mixed models to account for repeated measures with group, age and sex included as fixed effects. Alpha was defined as p<0.05.
Results
A total of 97 patients (49 outpatients and 45 inpatients) and 66 caregivers (43 outpatients and 22 inpatients) were enrolled. Patients had a median age of 59 years (range 18-71) and were predominantly male (60%) with 66% diagnosed with multiple myeloma and 34% with lymphoma. Majority of caregivers were spouses (76%). Inpatients were more likely to be employed and have lymphoma.
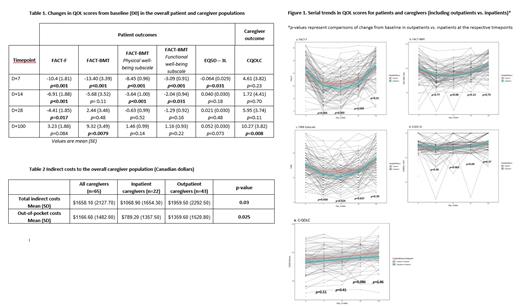
The overall cohort demonstrated a clinically meaningful decrease (≥4 points) from baseline in mean FACT-F scores (fatigue) at D+7, D+14, and D+28 with slight improvements at D+100 (Table 1). Compared to inpatients, outpatients overall exhibited significantly (p=0.011) greater changes in fatigue from baseline at D+7 and D+14, with comparable change scores at D+28 and D+100 between groups (Figure 1a). Moreover, for all patients, there was a clinically meaningful decrease from baseline in mean QOL scores by FACT-BMT (≥4 points) at D+7 and D+14, and a meaningful improvement at D+100, with no differences between groups (Table 1). On the FACT-BMT subscales, outpatients had overall worsening scores compared to inpatients on the Physical (p=0.029), and Functional Well-Being Subscales (p=0.043) (Figure 1c), while no differences were detected on the Emotional and Social Well-being scales. Health utility scores were also calculated from the EQ-5D-3L, with a significant downward trend in the overall sample at D+7; however, no clinically relevant changes (≥ 0.08) were noted, and results were comparable between groups (Figure 1d).
With respect to caregiver QOL, there were no differences in mean change scores between the two groups; however overall, caregivers had a significant improvement at D+100 compared to baseline (p<.05; Figure 1e). Outpatient caregivers experienced higher mean out-of-pocket costs ($1360 vs. $789, p=0.03) with the primary caregiver facing significantly greater total indirect costs ($1960 vs. $1068, p=0.025) (Table 2). For fully employed primary caregivers, the mean lost wages were $1231 for inpatients vs. $2150 for outpatients over the 3 month acute ASCT period.
Conclusions
There was significant deterioration of various measures of QOL in all patients, irrespective of outpatient or inpatient status. Outpatients, however, reported significantly greater changes in fatigue from baseline at D+7, D+14 and D+28. Caregiver QOL appears comparable between the two modalities. The financial burden on caregivers is high, with significantly higher total indirect costs in outpatient caregivers in the acute post-ASCT period.
Prica: Kite Gilead: Honoraria; Astra-Zeneca: Honoraria. Chen: Astrazeneca: Membership on an entity's Board of Directors or advisory committees; Beigene: Membership on an entity's Board of Directors or advisory committees; BMS: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Gilead: Consultancy, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy. Crump: Novartis: Membership on an entity's Board of Directors or advisory committees; Kyte/Gilead: Membership on an entity's Board of Directors or advisory committees; Epizyme: Research Funding; Roche: Research Funding. Kridel: Gilead Sciences: Research Funding. Kuruvilla: AbbVie: Honoraria; Incyte: Honoraria; Medison Ventures: Honoraria; Merck: Honoraria; Novartis: Honoraria; Gilead: Honoraria; Seattle Genetics: Honoraria; Karyopharm: Honoraria, Other: Data and Safety Monitoring Board; Roche: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; AstraZeneca: Honoraria, Research Funding; TG Therapeutics: Honoraria; Amgen: Honoraria; Pfizer: Honoraria; BMS: Honoraria; Antengene: Honoraria. Reece: Celgene: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; BMS: Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Sanofi: Honoraria; Millennium: Research Funding; Karyopharm: Consultancy, Research Funding; Amgen: Consultancy, Honoraria; GSK: Honoraria.